In our hospital, the diagnosis of Turner Syndrome is told to the girl and her parents together. Commonly, parents and their daughters have not heard of the syndrome nor know that it affects ovarian function. One study found that almost all parents (90%) find it difficult to cope with their daughter’s infertility. Published family stories and anecdotes show that parents are devastated by the information that normal ovaries are not present and that their daughter is unlikely to have her own child.
In my practice experience with families, the mother is shocked and often cries in the clinic consults. She thinks of the grandchildren she and her husband will never have. She mourns for her daughter’s future loss often well ahead of the daughter’s own sense of loss. The father is upset but may focus on his daughter’s external appearance ‘as long as she is happy and looks OK’, although he can grieve silently. Girls feel for their mother’s distress and may not wish to distress them further with questions about their own confusion.
At the age of puberty or when HRT is introduced, the doctor explains or re-explains to the girl that the ovaries will be unable to produce egg follicles, and that having babies ‘in the usual way’ is not possible. At the same time the doctor offers the girl and her parents encouraging information about alternative routes to forming a family, for example through in vitro fertilization (IVF) using egg donation or through adoption. One of my medical colleagues emphasizes to her adolescent patients the similarities they have with other young women – namely the ability to carry a pregnancy, give birth and breast feed. She may talk over the pros and cons of using a known or an unknown egg donor even at this early stage, but notes that her patients do not necessarily ask for further details until much later.
For some girls and parents, learning about the fertility status is more hopeful; 2–5 per cent of girls will have spontaneous menses and may have the potential to achieve pregnancy without medical intervention. For some others, infertility is more final; in approximately 6 per cent of girls one of the sex chromosome contains Y material and both gonads develop as rudimentary testes rather than ovaries, and are surgically removed due to the risk of malignancy. Healthcare pharmacy online – best place to order canadian medications.
At approximately age 16–18 years, most endocrinologists refer their patients to our hospital gynaecology clinic – which is staffed entirely by women – for more detailed discussion of fertility status, IVF and continuing review of health and older adolescent concerns. In particular the gynaecologist will gently explore issues over the next few years that may arise around relationships, sexuality and infertility. The gynaecology clinic consults with young women up to 24 years, thus offering a supportive transitional time before referral to the adult specialist or adult hospital clinic.
Neurotransmitters and Sexual Functioning
Cheapest viagra Australia
Sexual functioning is mediated and influenced, in a complex manner, by endocrine factors, neurotransmitters and neuropeptides.
The endocrine factors include androgens, estrogens, progesterone, prolactin, oxytocin, cortisol and pheromones. Neurotransmitters that are implicated in sexual functioning, mainly dopamine, serotonin and epinephrine, are also implicated in the pathophysiology of the major psychiatric disorders and in their pharmacological treatment.
Dopamine
Studies in humans and animals have suggested that the central dopaminergic system is involved in all components of male sexual behavior: desire, erection, orgasm and satisfaction. Dopaminergic agonists such as L-dopa, apomorphine, amantadine, bupropion and amphetamines have been reported to arouse sexual behavior while central dopaminergic blockers, like antipsychotics, suppress sexual functioning in both animals and humans.
Serotonin
Findings from animal studies suggest that 5-HT may facilitate, inhibit, or have no effect on sexual behavior, depending on which serotonin receptor subtype is involved. Studies on the effect of antidepressants on human sexual functioning suggest that activation of the 5-HT2 receptor impairs all stages of sexual response in males and females. Paroxetine, an SSRI, has been shown to be also a nitric oxide synthase inhibitor, and may diminish nitric oxide levels and function.
Epinephrine
Epinephrine inhibits erectile response in men, while blocking _1-receptors stimulates erection. By contrast, in women epinephrine facilitates vasocongestion while suppression of adrenergic activity impairs sexual arousal and orgasm.
Norepinephrine
Norepinephrine levels increase during sexual arousal in both men and women. The few studies that were done so far on this subject suggest that increasing the level of norepinephrine may facilitate erectile response in men.
Acetylcholine
Acetylcholine facilitates penile erection via the relaxation of smooth muscles of the corpus cavernosum. The role of acetylcholine in female vasocongestion is unclear.
Normal male sexual function is a constellation of processes: sexual desire or libido, the erection when the penis becomes firm, release of semen (ejaculation) and orgasm. Erectile dysfunction — commonly known as impotence — is defined as the inability to achieve or maintain an erection that is sufficient for satisfactory sexual activity. However, almost all men who have impotence can overcome it.
– Sexual desire, the release and expulsion of semen — emission and ejaculation — and the ability to have an orgasm occur via separate, distinct physical mechanisms. Due to a variety of reasons they can be dissociated from one another. For example, orgasm and ejaculation can occur without erection.
– Sexual desire or libido is determined mainly by the amount of testosterone in the body. As men get older the amount of testosterone that circulates slowly declines, decreasing libido. A decrease in libido also may result from depression and various medical problems that affect overall mental and physical well being.
– Ejaculation, the expulsion of semen during sexual activity, is affected by testosterone levels and medications as well as by the normal anatomy of the prostate and bladder. Decreasing amounts of testosterone, often occurring as a result of normal aging, will affect the volume of the ejaculate. Certain medications may also affect ejaculation. With aging, the volume of the ejaculate decreases.
– Surgery on the prostate or bladder and radiation can affect the amount of secretion produced as well as the ability to have normal ejaculation.
– Orgasm occurs as an experience of intense physical and emotional pleasure during the sexual act, and can occur separately and independently from erections, emission or ejaculation. Many factors, including emotional and psychological considerations, contribute to the experience of orgasm.
It is important to realize that male sexual function is defined by more than just the ability to have an erection. Mutually satisfactory sexual relationships can be maintained in the presence of impotence.
Chronic disease includes other cancer, hypertension, cardiac disease, diabetes or stroke.
Risk factors include antidepressant use, consumption of more than two alcoholic drinks per day, smoking, obesity, lack of exercise and watching television for more than 8.5 hours per week.
Impotence and Cancer Surgery or Radiation
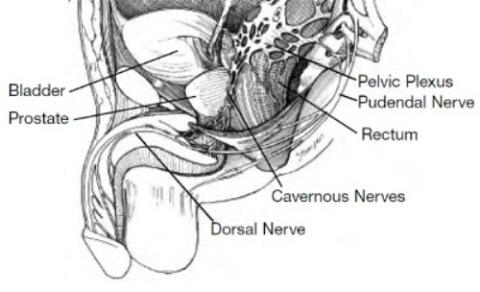
Impotence following major pelvic surgery or radiation, including prostate and bladder surgery, has been widely reported. During a radical prostatectomy the nerves which allow erection, called cavernous nerve bundles, and which lie within millimeters behind and on the side of the prostatic capsule, may be injured by being cut or separated from the prostate. This may cause temporary or permanent impotence, although sexual desire and the ability to achieve orgasm should remain. As discussed in Chapter Five: Other Causes of Impotence, radiation to the prostate, the bladder or rectum can damage the cavernous nerves as well.
The “nerve-sparing” radical prostatectomy or radical cysto-prostatectomy procedures to remove a cancerous prostate or bladder attempts to preserve these cavernous nerve bundles without compromising complete cancer removal. In the hands of an experienced surgeon, if both nerve bundles are spared, 50 to 90 percent of patients — depending on age and health — may have an eventual return of unassisted erectile function over time. When only one nerve bundle is spared, the percentage of patients that have return of erections over time is 25 to 50 percent. If a non-nerve sparing technique is used, the potency rate drops to 16 percent or less, depending on patient age.
Aside from the degree of nerve-sparing surgery performed, other factors are associated with impotence after radical prostatectomy.
- The biggest risk factor is age. Studies have shown that while the majority of men under 50 years of age are potent after radical prostatectomy, only 22 percent of men over the age of 70 are potent after the procedure.
- Other medical conditions that increase the risk of impotence include hypertension, smoking, diabetes, elevated cholesterol (hyperlipidemia) and heart disease. Depression, as well as other psychogenic factors, may affect psychological well being and recovery of potency.
- Unfavorable clinical and pathological stage of cancer also is associated with worse potency outcomes, as these men may not be candidates for a nerve-sparing approach because it may leave cancer behind.
It should be remembered that even if both nerve bundles are spared, with their proximity to the prostate (See Figure), these structures will likely suffer some injury that will take time to heal. Healing of the cavernous nerves and return of any unassisted sexual function may not begin until six months or more after surgery; however, it usually continues to improve over the next two to three years. Indeed a large percentage of men may not recover sufficient function for 18 to 24 months, some even longer. With prolonged disuse, the smooth muscles of the penis may atrophy, which worsens erections. Early and aggressive treatment of impotence with oral or injection medication may improve and speed up recovery of erectile function.
For men undergoing radiation, the amount and extent of radiation as well as whether or not they are treated with hormone therapy correlates with the likelihood of impotence, either temporary or permanent. The reduction in libido and possible difficulties with erections from the use of hormone therapy is generally reversible when the therapy is discontinued. The likelihood of irreversible effects is related to patient age, pre-treatment sexual function and the length of time hormone therapy is given.
Even if impotence is present after surgery or radiation alone, the ability to achieve an orgasm should remain. However, with the prostate removed there is no ejaculate although some secretions may remain. During orgasm, there is no emission or expulsion of semen. The ejaculate volume will decrease with radiation as well.
Anxiety is an important factor in the development of sexual dysfunctions. The phenomenon of performance anxiety is well known, particularly in men who are concerned over their erectile response and durability of the erection. Narcissistic perturbation is yet another psychological consequence of ED that further increases anxiety. The patient’s self-esteem may sink further causing concern for both himself and his partner. This may result in behavioral modifications in the patient, such as avoiding intimacy and temper outbursts. These lead to increasing anxiety and increasing ED resulting in a vicious cycle of failure and escalating anxiety. This specific situation can be treated in most cases with the help of explanations and short-term therapeutic intervention intended to relieve anxiety.
Roughly 15% of the population suffers from various kinds of anxiety disorders. Those include generalized anxiety disorder, panic disorder, obsessive-compulsive disorder (OCD), social phobia (SP) and posttraumatic stress disorder (PTSD).
Research, dating back to the 80s, shows that people with high levels of anxiety have a higher rate of sexual dysfunctions. Although the psychoanalytic literature has directed much attention to the association of anxiety provoked by intrapsychiatric conflicts and sexual dysfunction, there is little information on the comorbidity of sexual dysfunction and anxiety disorders. Kaplan claimed that the role of anxiety is especially clear in the pathogenesis of sexual aversion disorders and phobic avoidance of sex. She found an unexpectedly high incidence of panic disorders in patients who phobically avoid sex or who complain of active sexual aversion. Some of the patients actually experienced panic about their sexual performance or became obsessed with details concerning their sexual performance and loss of control. Monteiro et al. found a high percentage of sexual pathology in untreated patients with OCD of whom up to 24% were virgins and another 9% had not had sex for years.
SP and Sexual Behavior
The main component of SP is extreme fear of public behavior that may cause embarrassment or ridicule. This is a combination of performance anxiety and interpersonal anxiety that exists in 7% of the population. It is reasonable to expect that this type of anxiety disorder is accompanied by sexual dysfunction. Heimberg and Barlow hypothesized that sexual dysfunction (especially reduced erectile capability) is a result of performance anxiety or fear of scrutiny by others, similar to SP. Using a laboratory model, they found that healthy men exposed to both erotic stimuli and anxiety-provoking stimuli showed increased arousal compared to healthy men exposed to erotic stimuli alone. However, in sexually dysfunctional males, the opposite occurred: they reacted to the anxiety-provoking stimuli with decreased arousal. The authors concluded that anxiety apparently affects sexually functional and dysfunctional males in opposite ways and that dysfunctional males may employ the same cognitive model as patients with SP. There are several studies suggesting that patients with SP may have sexual problems. In a study of college students, Leary and Dobbins reported that subjects with a high rate of ‘heterosocial anxiety’ showed a higher incidence of sexual dysfunction. Figueira et al. reported a 33.3% rate of sexual difficulties, especially premature ejaculation, in patients with SP. Bodinger et al. evaluated 40 consecutive, drug-free outpatients with SP (24 males, 16 females) attending an anxiety clinic, and 40 healthy, age and gender-matched controls. A detailed rating scale was used to assess quantitatively and qualitatively sexual function and behavior. The findings showed that men suffering from SP reported moderate impairment in sexual enjoyment and subjective sexual satisfaction. In addition, the men reported a later age for first sexual experience and a higher rate (42%) of paid for sex as compared to the healthy men (8%). Women suffering from SP reported severe impairment in desire, arousal, sexual activity and subjective satisfaction. These women had less sexual partners compared to the healthy controls. Seven out of 16 (44%) had only one partner or none throughout their lifetime, compared with 6% in the control group. Both men and women showed avoidance of intergender behavior. Viagra in Canada – ed medications with great discounts.
PTSD and Sexual Disorders Exposure to extreme traumatic events (military, traffic accident, rape) may lead to behavioral and physiological abnormalities which at times persist long after the precipitating event and become permanent, leading to the clinical syndrome known as PTSD. PTSD is known to affect significantly emotional, social, occupational and sexual functioning. Kaplan has shown that sexual problems are prevalent among PTSD patients. Letourneau et al. reported that over 80% of PTSD patients studied, were experiencing clinically relevant difficulties. ED and premature ejaculation were the most frequently reported problems. They suggest that PTSD may be a risk factor for sexual problems. PTSD patients are frequently treated for symptoms of anxiety and depression, mainly with anxiolytics and antidepressants. Fossey and Hamner reported that clonazepam can cause sexual dysfunction in male veterans with PTSD. The role of antidepressants in inducing sexual dysfunction is well known.
A study by Kotler et al. compared the various components of sexual functioning among three groups of males:
- untreated PTSD patients (n _ 15),
- PTSD patients being treated with SSRIs (n _ 27)
- a group of healthy controls (n _ 49).
All participants completed an 18-item questionnaire for assessment of sexual functioning. Those with PTSD also completed the impact of events scale and the symptom checklist-90. Untreated and treated PTSD patients had significantly poorer sexual functioning in all domains (desire, arousal, orgasm, activity and satisfaction). Compared to healthy controls, those treated with SSRIs had greater impairment in desire, arousal and frequency of sexual activity with a partner. There was a high correlation between sexual dysfunction among the PTSD group and the anger-hostility subscale of the symptom checklist-90.
Treating male PTSD sufferers with sildenafil in a dose of 50mg brought about significant improvement (53.5%) in erection functionality and at the same time improved desire, orgasm and sexual satisfaction. This study shows that the phases of the sexual cycle are connected to each other and improving one usually results in improvement of the other phases. In conclusion, anxiety disorders are associated with a significant impairment in all domains of sexual functioning.